Euploidy and Euploid Embryos: A Plain English Guide For Women Aged 38+ In 2025
There is almost nothing more important for a woman who is 38-40 or older starting out or continuing IVF, than understanding what a euploid embryo is and the factors that impact your euploidy rate. Why? Because your chance of bringing home your baby after three to five euploid embryo transfers is 93-99%, while three aneuploid transfers will deliver you a chance of less than 1%.
You will face unique challenges in your IVF journey. And one of the most difficult of these is the fact that by virtue of your age (regardless of how fit and healthy you are), your chances of having a baby are lower. This changes how the system treats you, how your body responds and whether or not you achieve your dream of becoming a parent.
I have been where you are and this is the euploidy guide I wish I had had when I started IVF for the second time at age 39. Everything I learned from that point onward, I applied rigorously until I shifted by own euploidy rate and ultimately have my first euploid transfer end in a successful ongoing pregnancy.
This guide is made to cover everything you need to know about euploids, in a way that is hopefully a lot more plain english than you’d get just by diving into . And a lot more in depth than the basics that most IVF clinics have on their websites. I also include links every relevant statement or insight to reputable sources and studies so that you can investigate and interrogate the data yourself if you wish.
Understanding Euploidy and Preimplantation Genetic Testing (PGT-A)
Euploidy is how we refer to an embryo that is euploid: an embryo that has exactly two copies of each of the 23 chromosomes that humans have. No more, and no less on any one of the 23 individual chromosomes.
Unlike every other cell in the body (somatic cells), “gametes” (female eggs and male sperm cells) hold only half of the genetic code required for life—that is, 23 chromosomes each. Through the process of fertilization, these 23 chromosomes come together to create 46 in total. In biological terms for humans at least, each of these pairs are called “homologous chromosomes” – meaning a basic chromosome number of two: one from the biological mother and one from the biological father.
There is no way of knowing whether an embryo that is created in vivo (that is, through the process of sexual intercourse and natural conception) is euploid or not. This is a concept that has only come to be understood through IVF and a process of testing called “PGT-A”: preimplantation genetic screening for aneuploidy – i.e. abnormal cells contained within an embryo which allows embryologists to identify euploid embryos and prioritise them for transfer ahead of other options.
How is a euploid embryo created?
A euploid embryo is created when the process of mitosis (where the fertilized oocyte, i.e. the egg, begins to divide) occurs without errors. For this to happen, the spindle within the oocyte which contains the genetic code needs the perfect environment for the cell division process to occur.
For instance, enough energy needs to be being produced by the mitochondria within the oocyte, the spindle itself needs to be nicely aligned, and the motor neurons that physically help to pull on the edges of the spindle in order to split the chromosomes need to be working at their peak.
One mistake, and a chromosome may have more than two copies (trisomy or polysomy), or it may be missing one copy (monosomy). Without balanced genetic material, the risk of miscarriage or birth with genetic disorders increases, while a nice, even division between daughter cells is what creates a euploid embryo. This can sometimes also in medical literature be referred to as “diploid” which just means the cells have two complete sets of chromosomes (2n).
Why does euploidy matter?
Euploidy matters—particularly for women over 38—because your chances of producing a euploid embryo with in vitro fertilization decrease as your age increases. And a euploid embryo gives you the greatest chance of taking home a live baby.
This is a process of decreasing chance is gradual. It doesn’t immediately happen at 35 or 38. It is a decline that appears to begin from approximately age 33 for women. Unfortunately it is also individual. While the statistical averages tell one story, there are of course many individual cases of younger women who struggle to produce euploid embryos.
Ultimately this is what is meant when people say “fertility declines with age”. It means that as a woman, you can still have a period, you can still be capable of getting pregnancy, but the likelihood of any pregnancy resulting in a live birth gets lower and lower. Another way of putting this is that over 38, with a natural pregnancy, the chance of miscarriage increases until by age 45-48, that chance may increase to 80-95%.
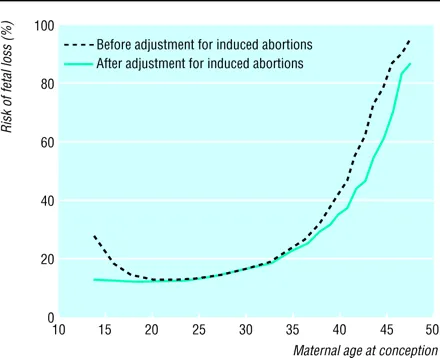
Source: BMJ, 2000 (Maternal age and fetal loss: population based register linkage study)
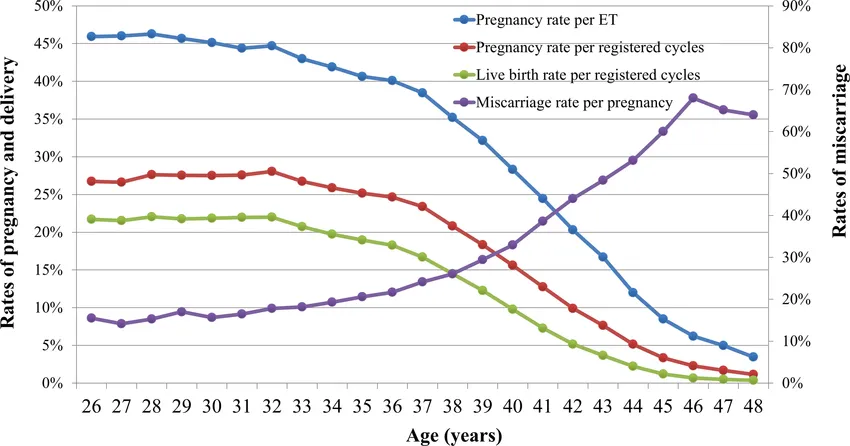
Source: Reproductive Medicine and Biology, 2021
A similar decline in fertility occurs for men from a similar age, and although it is less pronounced, it can significantly impact IVF outcomes for women who are already older.
How does age affect the probability of producing at least one euploid embryo per cycle?
As your age increases, the probability of producing at least one euploid embryo within any given IVF cycle is reduced by these key things:
- Your age
- Your AMH (Anti Müllerian hormone – a measure of your ovarian reserve – the number of oocytes you have remaining)
- Your antral follicle count (the number of baseline follicles in your ovaries before you start IVF medication)
- And often as a result of the three things above, the number of blastocysts you’re capable of producing
Unfortunately as women age, their AMH decreases, as does their antral follicle count. As a result, less eggs are collected and therefore less embryos can be produced.
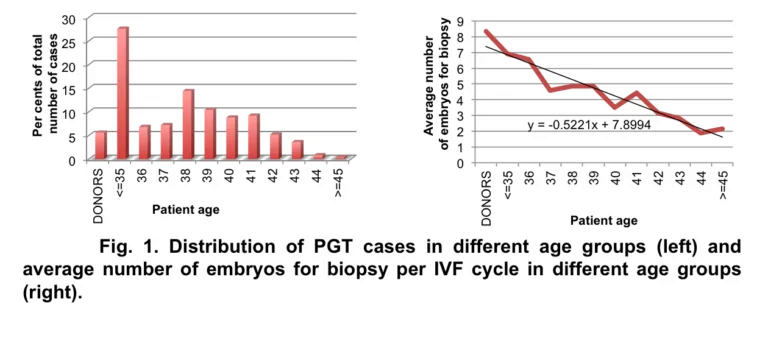
In addition, these impacts of age impact aneuploidy rates and euploidy rates: which means the percentage of total embryos from any given cycle that are found to be euploid upon testing.
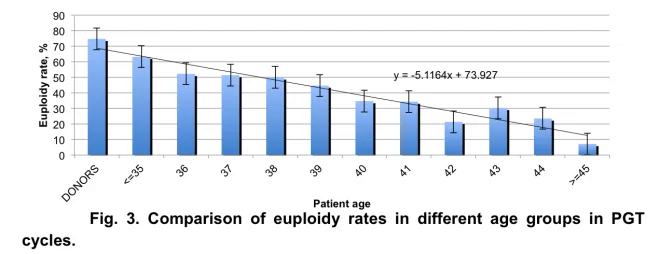
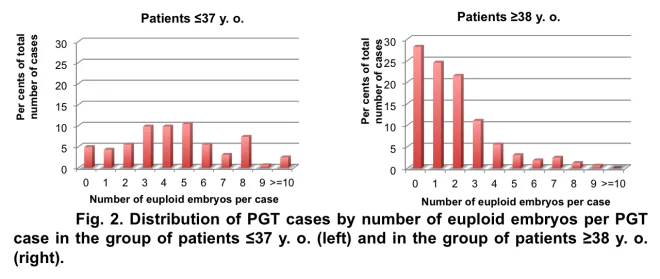
So let’s say you’re 41 and you produce 1 blastocyst. The likelihood of that embryo being euploid is approximately 30%. Another way of putting it this is: you may only get a euploid embryo one in every three cycles – or three of you may be unlucky and get none, while seven other women get one. But let’s say you produce 7 embryos. In that case, a 30% chance could mean you end up with 2 euploid embryos despite your age. In essence, your chance of producing a euploid is a higher the more embryos you produce, but it is not guaranteed either way.
What if you don’t produce even a single euploid embryo in your first IVF egg retrieval cycle?
This is unfortunately very common for older women to experience and it’s something that gets asked in IVF forums a lot. A single cycle can cost up to $30,000, so the fact that something which costs so much can fail to produce a single high opportunity for a baby is devastating. Many women rightfully want to know: if they didn’t produce a euploid within their first cycle, what are the chances of producing one in subsequent cycles?
There has been research that has looked at this. The graph below shows that at 41-42, 43% of people who did not get a single euploid in their first cycle will produce one in their second. But over 42 that figure drops to 13%. In short though, your chances effectively remain the same across a second cycle (the same as what is standard for your particular age).
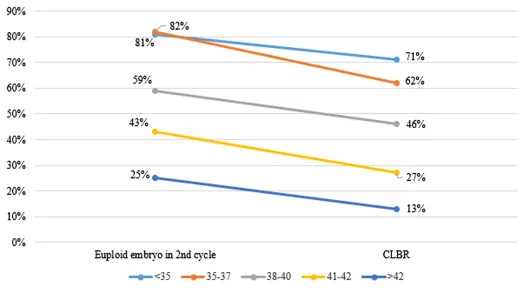
Source: Fertility and Sterility, 2022
Is it worth doing multiple cycles to produce a euploid embryo
There is a belief within the IVF community for older women on Facebook and Reddit, that “it’s a numbers game.” While this is true to a certain extent, certainly for the first couple of cycles, especially beyond age 42, this is no longer the case.
What the below graph shows is that there is really a maximum amount of cycles in which it makes any sort of logical sense to continue with extra cycles with the belief that doing so could result in an increased chance of a successful pregnancy:
- 5-7 cycles age 43 to 46 (but a less than 1% extra gain for doing more than 3 cycles)
- 3-4 cycles age 47-49 (but a less than 1% gain for doing more than 1 cycle)
However if you read the cumulative live birth rates, it tells a rather depressing story:
- At 43, out of every 100 people, it takes 7 cycles to achieve the maximum possible live birth rate of 9.5 women out of that 100 people
- At 44, this drops to 8.5 out of 100
- At 45, this drops to 5.5 out of 100 (95 women out of every 100 fail)
- At 46, this drops to 4.5 out of 100
- At 47-49, this drops to 1-3 out of 100 (97-99 women out of every 100 fail)
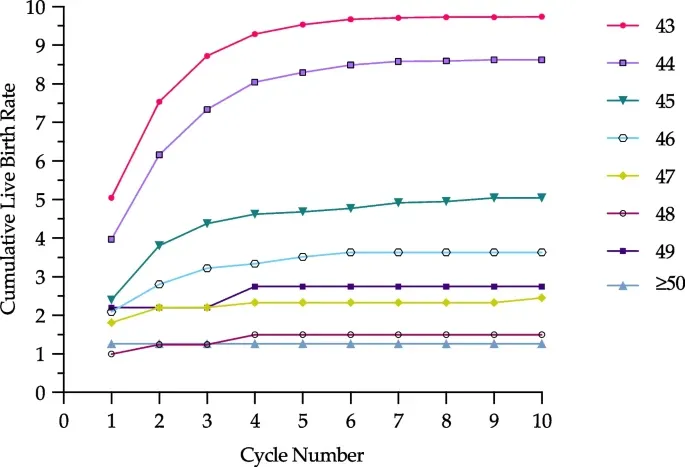
Source: Reproductive biology and endocrinology, 2023
So the answer to this question is: it depends. This research gives you a clue as to how many it may make sense to do (if you can financially afford it), but what no research study is going to do is understand or speak to your personal circumstances.
Understanding how to read research when with or without euploid embryos
The thing that older women need to be aware of when reading IVF research in general is:
- Not all IVF research is done on older women – in a significant amount of cases there are many more research participants who are under rather than over 35 which can also skew the averages that we see in results. And in some cases, the results are not broken down by age making it difficult to draw conclusions about how something works for older women.
- Lots of research, because of the number of participants in a study, needs to group age brackets together, which might give a false sense of what to expect. For instance if you group everyone under 37 and everyone 38+, then the results from people who are 38 to 40 are going to make the results from people in the study aged 41-50 look better than they in fact would be when broken out year by year. Where possible, you need to find research that best represents your specific age.
Once you understand these things, you can begin to read IVF research with a much more critical eye, and one that can pick out new research that relates to you based on your age anything else that may be unique about your personal situation (some of the ones that are regularly studied separately include: Good prognosis patients with high AMH levels or antral follicle counts, DOR – diminished ovarian reserve, PCOS – Polycystic Ovarian Syndrome, RIF – recurrent implantation failure, RPL – recurring pregnancy loss and various sperm related issues).
What’s the difference between euploidy, aneuploidy (triploidy, monoploidy, polyploidy) and mosaicism?
First, a bit of context. As a result of the recent lawsuits filed in the US against testing companies such as Cooper and Igenomics, there has been increasing levels of misinformation circulating within the IVF communities on social media for older women. These can usually be summarised as:
- A strong belief that the testing process is complete incorrect (while there can be either test errors in the range of 1-3% or differences in concordance rate up to 15% (what the placental cells which are tested say vs what the actual cells that become the baby say), this ultimately does not change the reality of live birth rates for older women.
- A strong belief that somehow whole chromosome aneuploid embryos can “self correct”. It is more likely in cases where aneuploid embryos do result in the live birth of a healthy baby (which can and does occur in very small numbers of cases), that
Where these beliefs lead to people choosing not to test and therefore to not consider any alternatives or ways of improving their euploidy rate, it is possible they do themselves a disservice. While this is still a hypothesis that has not been verified, younger women are much more likely to experience a scenario where the placental cells do not match the ICM (inner cell mass – the cells that become the baby) and to be successful with the transfer of a whole chromosome aneuploid embryo than is a woman aged 40+. Think in the order of 5% for this younger cohort versus less than 1% chance for older women.
That being said, euploidy itself is a spectrum. And that spectrum is defined by the laboratory cut offs which are designated by the big testing companies (Cooper, Igenomics and so on).
In the most recent half of the last decade, it has become commonly accepted within many IVF clinics that just because the placental cells of an embryo does not test as euploid (as per those cut offs), does not mean the embryo has no chance of ending in the birth of a healthy baby. Enter: the power of mosaicism.
But first let’s back up a bit and revisit some of these definitions for clarity:
What is a euploid embryo?
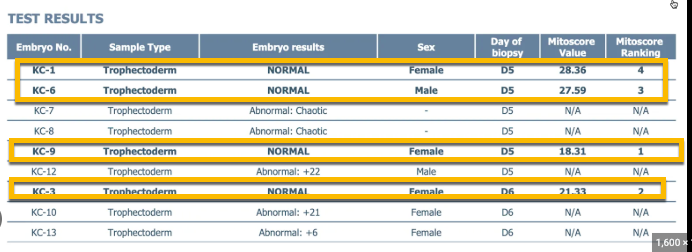
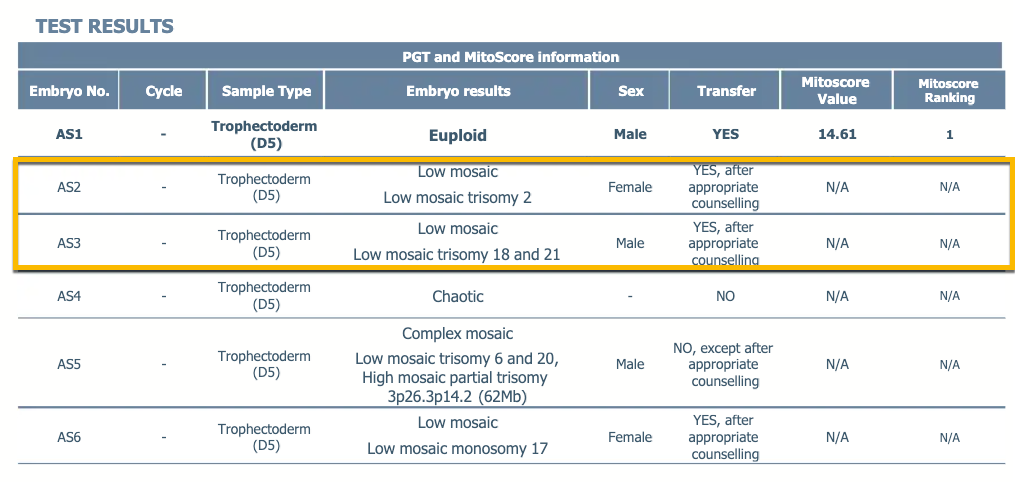
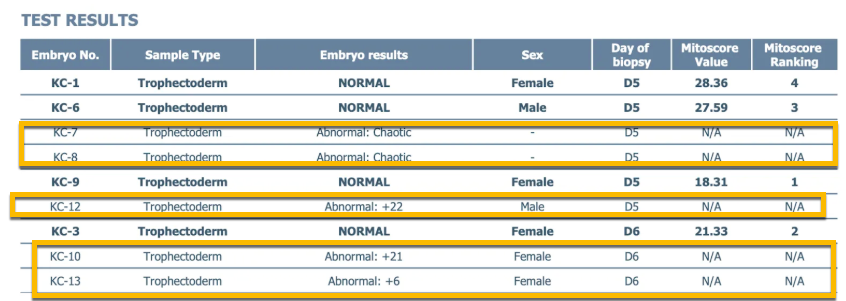
As a reminder, a euploid embryo is an embryo where 20%-30% (depending on the lab) or less of the placental (trophectoderm) cells from the embryo’s outer layer that were tested had missing or additional chromosomes. Each chromosome is “diploid” which means it has the exact multiple of 2 x 23 chromosomes: one from the egg and one from the sperm. PGT-A test results will look something like this:
The correlation between embryo quality (that is, it’s morphological qualities that are scored by using a grading method such as Gardner or Schoolcraft) and the likelihood of an embryo being euploid decrease with age. As you can see in the graph below, having an AA grade embryo still only gives a 43 year old woman a 40% chance that the embryo will be euploid, unlike a 90% chance at age 26, or a little less than 80% at age 30.

Source: Archives of Gynecology and Obstetrics, 2021
What is a mosaic embryo?
An embryo is considered mosaic when between 30% and 70%/80% of the cell speciman tested are abnormal. Usually chromosome sets between 20%-49% are considered “low level mosaic” while 50%-70%/80% are considered “high level mosaic”. Like aneuploid embryos, mosaic chromosomes can be either triploid (have three copies) or monoploid (have only one copy) – the main difference is the percentage of cells impacted is lower. PGT-A test results will look something like this:
A landmark study conducted in 2021 where 1000 mosaic embryos were transferred, used this data to create a new hierarchy to help doctors help their patients select which order embryos should be transferred in to confer the greatest potential for live birth.
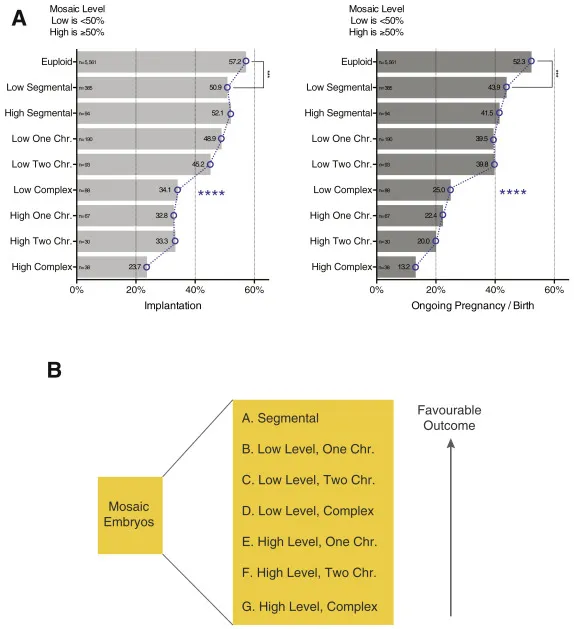
Source: Fertility and Sterility, 2021 (Using outcome data from one thousand mosaic embryo transfers to formulate an embryo ranking system for clinical use)
Understandably is often a level of fear around potential chromosomal disorders that may result from the transfer of mosaic embryos, and different clinics have different levels of tolerances that their genetic counsellors may position with patients, however it should always be remembered that thousands upon thousands of untested embryos are transferred every day – many of which would be mosaic, and within the literature of known mosaic transfers, the occurrence of children born with mosaicism is around 1 in 1,000 – about the same as you would have if you got pregnant naturally in your early thirties. NIPT testing at 10-13 weeks can help determine further risk for patients who wish to transfer mosaic embryos.
What is an aneuploid embryo?
An aneuploid embryo is an embryo where more than 70% or 80% (depending on the lab) of the placental cells tested had missing or additional chromosomes. In other words, they have abnormal cells which results in an abnormal number of chromosomes – the correct number being two. On PGT-A reports, aneuploids often referred to as abnormal. Aneuploid embryos can also be triploid or monoploid, and they can also be “polyploid” which in the context of IVF is used to mean more than triploid–i.e. more than three copies.
An important thing to note here is that a few less well known companies (such as Progenesis), have shared with private patients that their cut off rates for aneuploidy are much lower than others (this is not stated by the company publicly).
This is a scenario where it is imperative that women know who the lab provider is, and even request original results so they can understand the exact percentage rather than the reported interpretation because there are significant differences in live birth rates possible between a whole chromosome aneuploid as understood by the biggest labs (70-80%) and a mosaic embryo (20/30%-70/80%).
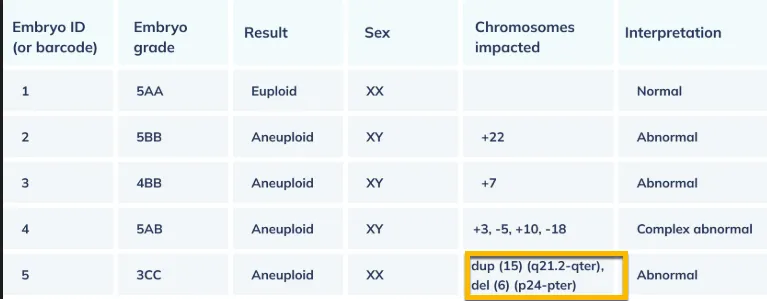
While the 2021 Viotti study did not transfer any segmental aneuploids, recent research continues to emerge these specific types of aneuploid embryos (those embryos that have 70-80% or greater of a particular segment of a chromosome deleted or duplicated) have around a 20-24% chance of live birth. This live birth rate makes segmental aneuploids actually better options than complex mosaic embryos.
A segmental aneuploid result looks something like this on a PGTA test result:
Unfortunately for many women over 40, they’re not getting mosaics or even segmental aneuploids. The majority are getting whole chromosome aneuploids and often embryos with not just a single chromosome impacted, but multiple.
There are bigger studies in progress that is looking at the outcomes related to transferring known “whole chromosome aneuploid” embryos. This means, not segmental, but where a complete chromosome has lost 70-80%+ of a copy or added 70-80% of an extra copy.
Since 2020, 4 studies (see my summary here) have looked at whole chromosome aneuploidy transfers using Next Generation Sequencing – the tool that is used to complete pre implantation genetic testing. I personally reviewed thee studies and calculated a total of 252 transfers of whole chromosome aneuploid embryos completed.
Not all of thee studies reported the flow from transfer to implantation to clinical pregnancy to live birth, but overall, there were 3 reported live births from all 252 transfers. This gives you an initial idea of just how much lower the chances are with a whole chromosome aneuploid. No age breakdowns were provided either which means we don’t necessarily know whether any of these live births were to women over 38.
Once an embryo is tested, many clinics will refuse to transfer . Or even if they do allow for aneuploid transfers, there may be certain specific genetic disorders that they will not transfer due to the fact that the disorder is survivable (such as down syndrome – a type of aneuploidy that results from an extra chromosome 21, XXX – a type of aneuploidy where a chromosomal female has an extra copy of chromosome 23, or Turner Syndrome where a chromosomal female is missing a copy of chromosome 23). In essence, “survivable” means there is a better than 1% chance (often 20-30%) that you could carry baby with a known genetic disorder through to a live birth.
Euploid Success Rates and Outcomes
What are the chances of pregnancy or live birth with a euploid embryo that you produced yourself (at a similar age to transferring it)?
It is relatively well accepted that for the most part, once a euploid embryo is produced, there is a much more reasonable chance of a live birth. But ploidy status isn’t the only determining factor of success. The number of days that an embryo takes to reach blastocyst stage (5, 6 or 7 days), embryo morphology (how it looks) and its expansion also contribute to the probability of implantation and live birth. However, the data that had been available until relatively recently only broke down outcomes through to age 39 or 40.
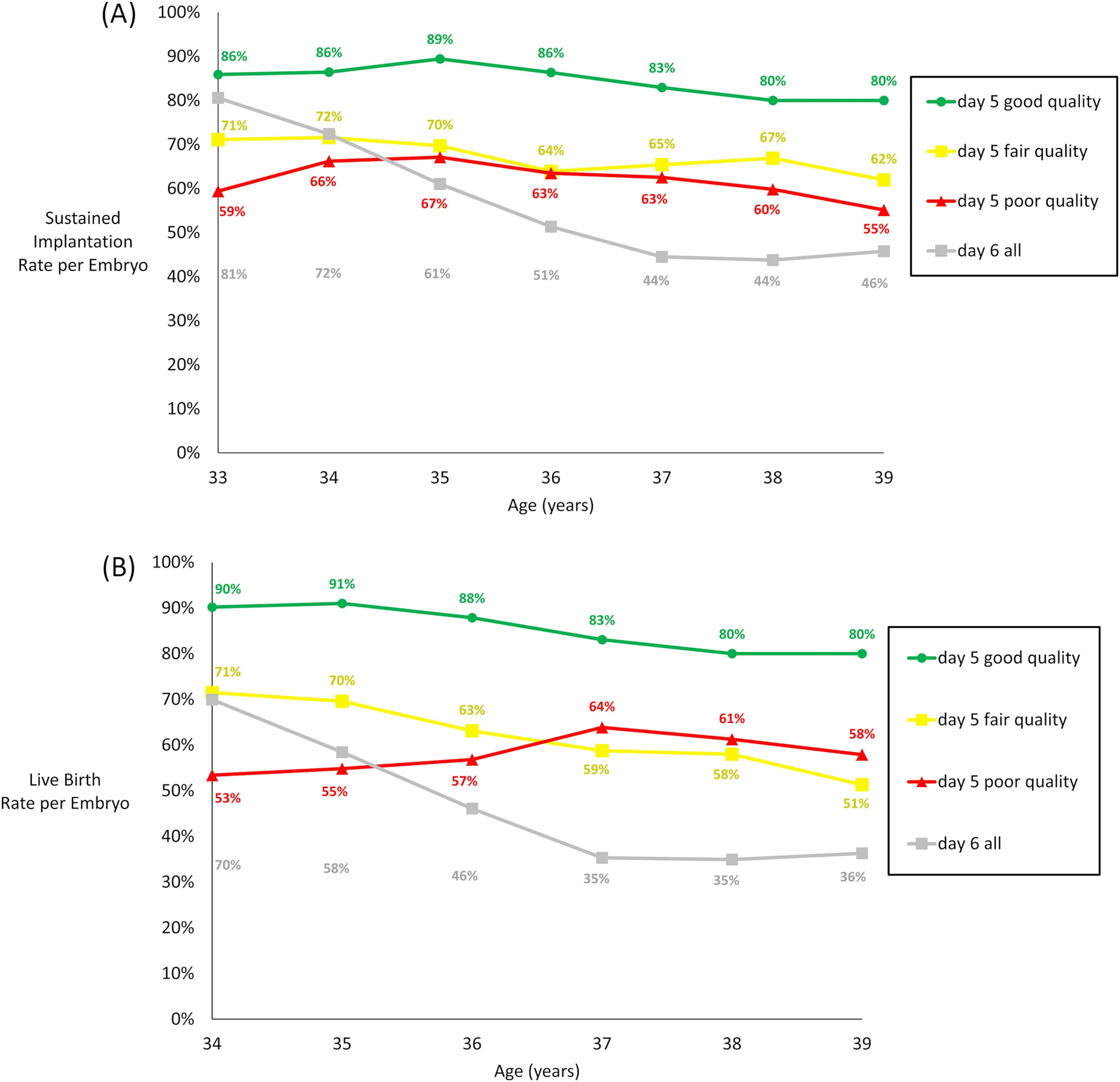
Source: Reproductive Biomedicine, 2021 (showing sustained implantation rates and live birth rates
Even as recently as 2025, studies have been released showing ages 38+, while having a lower chance of live birth with a euploid are still significantly better (40%) compared to when you look at overall averages. But again, the problem here is the data is not being broken down by the older age brackets.
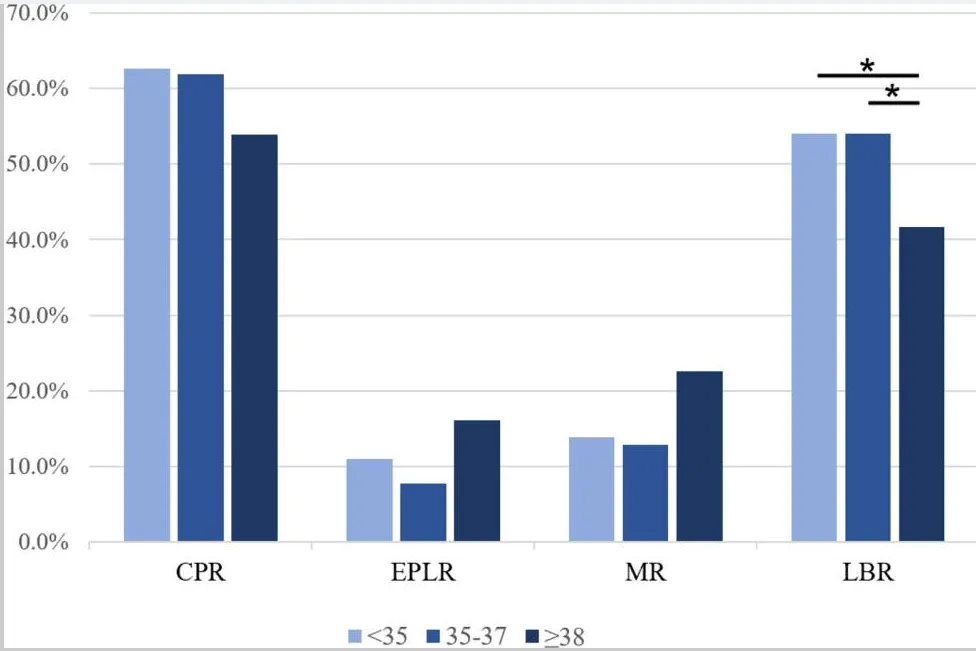
Source: Journal Ovarian Res, 2025
The most recent study to do this was 2025, and it showed a poorer picture. It found that qhile the age of the oocyte was not in fact of concern (there was not significant ), for instance of a 45 year old woman happened to produce a euploid embryo and then transfer than embryo into a surrogate, then the likelihood of live birth would be the same as a euploid embryo produced by a younger woman.
In contrast however, woman’s age at transfer (<38, 38–42, 43–45, >45 years) did begin to impact the success of euploid embryo transfers, especially from 43 onward. Still, having a 40% chance of live birth at age 45+ when we consider the fact that looking at general results the average chance would be 3%—is incredible.
- Age <38 (57.1%)
- Age 38–42 (58.7%)
- Age 43–45 (50.0%)
- Age >45 years (40.5%)
Source: Annual meeting of of the European Society of Human Reproduction and Embryology, 2025
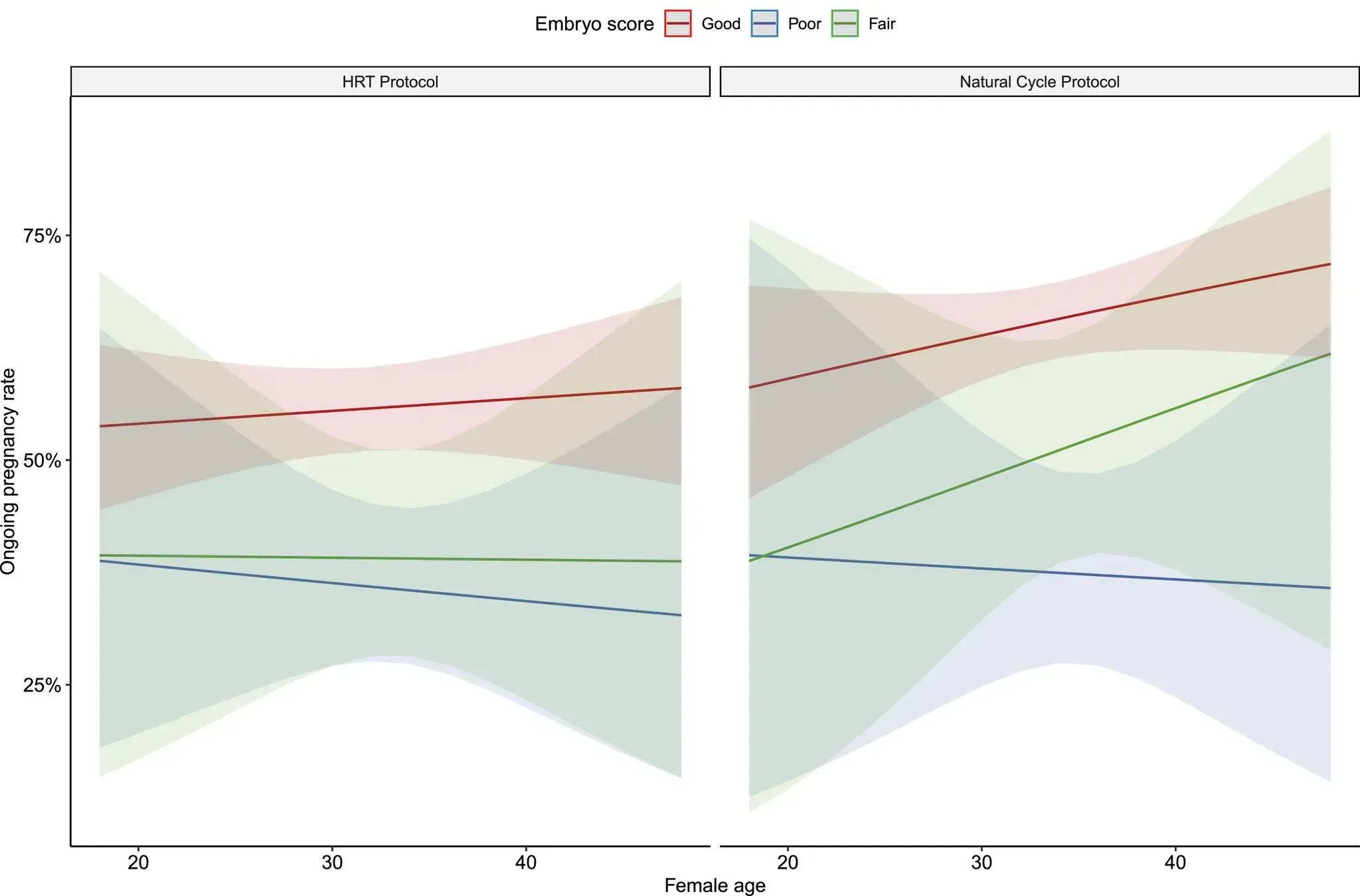
Interestingly there is also new research emerging in this area to show that live birth rates for euploid embryos can be further impacted by the type of endometrial preparation used (either natural or medicated). The common consensus being formed is that natural produces better live birth outcomes but it wasn’t until 2024 that a study appeared to show the same thing broken out for older cohorts.
This large retrospective study examined 1,923 single euploid frozen embryo transfers matched by morphology, comparing natural cycle (NC-FET – “Natural Cycle Frozen Embryo Transfer”) to hormone replacement therapy (HRT-FET “Hormone Replacement Therapy Frozen Embryo Transfer”). 216 of them were over 40 years old and 94 of these had an ongoing pregnancy.
For women who had a regular cycle, the natural cycle protocol produced significantly better ongoing pregnancy rates than the hormone replacement therapy protocol.
Of course, clinics have long preferred HRT because it allows them to control the timing of your cycle and reduces their administrative burden. But we are now coming to understand than these appear to be directly trading off on the number of women who bring home a live baby from the precious euploids they worked so hard to produce.
What are the chances of a miscarriage if you transfer a euploid embryo?
The truth is that unfortunately euploid embryos can still miscarry (approximately 13-15%, depending on the study), although at a much lower rate than mosaic and aneuploid embryos which have chromosomal abnormalities.
SHOW MISCARRIAGE RATES FOR MOSAIC AND ANEUPLOIDS HERE
Giving your body the best chance to carry a euploid embryo to term comes down to ensuring that your uterine environment is as optimal as it can possibly be.
According to this research study in the Sept 2021 edition of Fertility and Sterility, after euploid FET (frozen embryo transfer) loss, most could be explained by abnormal endometrial factors (45%) and abnormal genome (12%), but 38% remained unexplained.
My personal hypothesis (not verified by research), is that the more euploid embryos you have in your cohort of embryos, the more likely your euploid result is accurate, therefore the less you have to worry about the 12% abnormal genome factor.
Another research study also found there are certain risk factors that can increase the possibility of you being in that 13-15%—specifically your BMI and your number of previous miscarriages. While the latter is not controllable, the former provides some level of control that can be asserted prior to transfer, especially with the increasing access to GLP-1 drugs such as Ozempic and Wegove.
What is the cumulative live birth rate after multiple transfers of euploid embryos?
Some great research has been done in this area especially since 2021. The first major study released in this area found that after three successive frozen embryo transfers of euploid embryos, that the live birth rate was 92.6%!
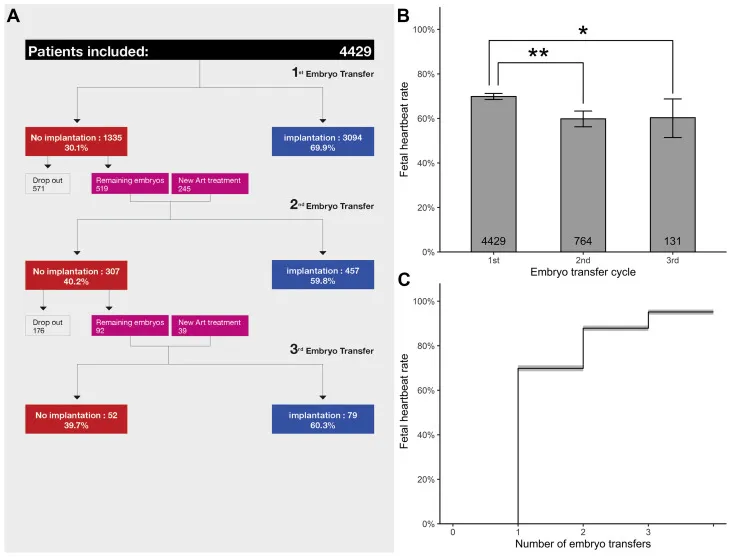
And then a follow up study was conducted to really test the theory and in looking at over 123,000 patients with over 64,000 euploid blastocysts transferred, that the fourth and fifth euploid embryo transfer resulted in 96.5-99.6% chance of live birth
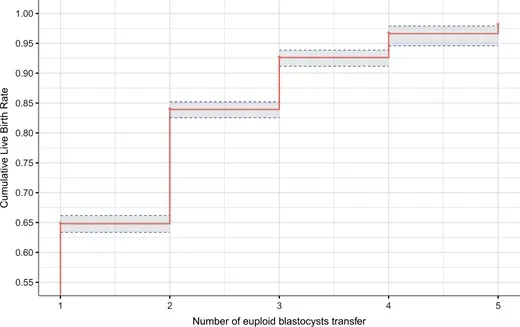
In other words, if you can produce 3-5 euploid blastocysts, you are almost guaranteed to take home a live baby.
Of course, for women in the 38+ age bracket, sometimes the ability to produce a single blastocyst for testing is hard enough, let alone one euploid, let alone five. So while this is good news for those who can produce euploids, it does not ultimately change the outcome for older women unless they are actively working on methods to shift their euploidy rate through the use of experimental techniques and add ons.
And further, for older women it would not be good enough to have even one euploid embryo fail when in all likelihood this may be your only euploid. Euploids are so precious, every possible failure point for implantation and ongoing pregnancy should be investigated before transfer occurs.
This post is to be continued. When I add to it next I’ll cover the following topics:
Producing a Euploid Embryo at 38+
- How many eggs are typically needed at age 38+ to achieve at least one euploid embryo?
- What are the male partner or male donor contributing factors to euploidy?
- How can women of advanced maternal age increase their chances of producing a euploid embryo?
- How can women with low AMH increase their chances of producing a euploid embryo?
- How do stimulation protocols (e.g. microflare, dual stim, mild stim) affect the likelihood of producing a euploid embryo?
- Can supplements or lifestyle changes improve the chances of a euploid embryo?
Beyond the Basics
- I just got a euploid embryo! How likely is it that the test results are incorrect?
- How likely is it that the inner cell mass is euploid even if the trophectoderm is not?
- Do higher-grade blastocysts have a greater likelihood of being euploid?
- Is it better to bank multiple embryos before testing for euploidy?
- Does the uterine environment impact the success of a euploid embryo transfer?

Author: Michelle Bourke
Founder, Better IVF